They made their bed – and were forced to lie in it.
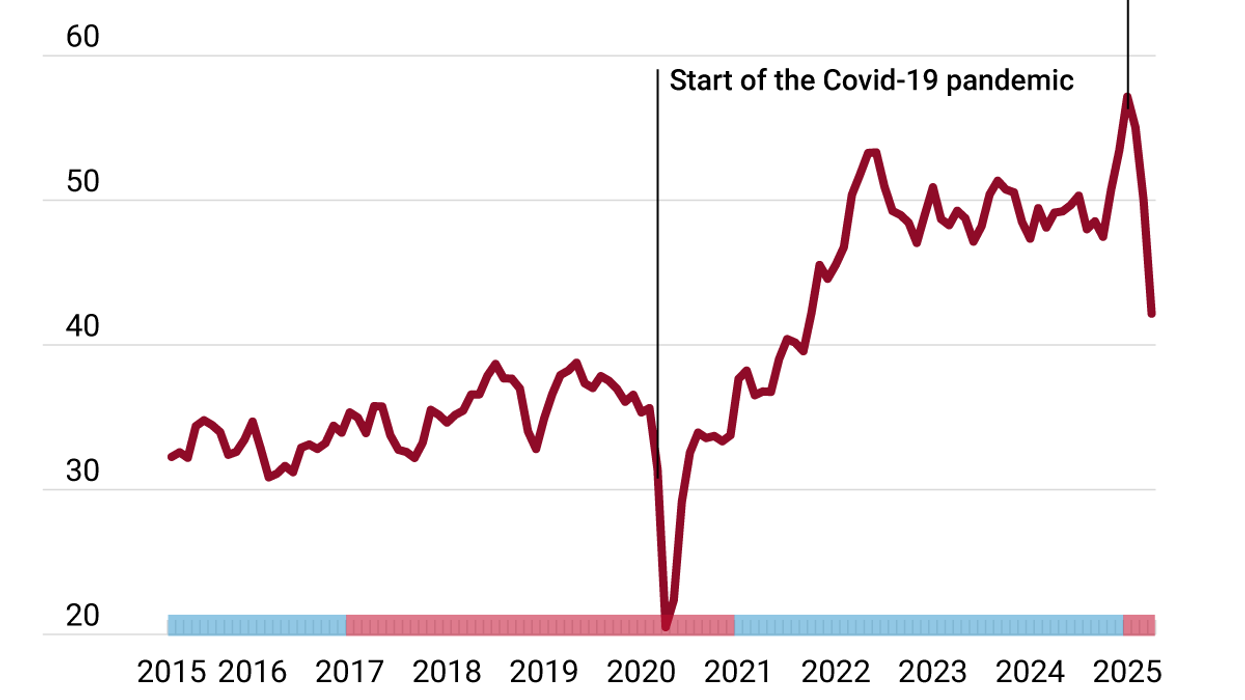
At the start of the pandemic, G7 countries were plagued by a huge uptick in hospital admissions – and the shocking reality that hospital beds had been on a 50-year decline. Four years later, these countries have still not reversed the downward spiral.
In the US, over the last five decades, care has shifted away from inpatient hospital settings and to outpatient services to cut costs. The decrease has also been intentional. In 1974, the government began an initiative to directly cut the number of hospital beds, believing in a rule called Roemer's Law, which said that “a hospital bed built would be a hospital bed filled,” thus driving up costs.
However, the US’s free-market healthcare system still provides more hospital beds per capita than the government-dominated system in Canada. According to the Canadian Institute for Health Information, Ontario has just one intensive-care bed for every 800 residents, giving it no surge capacity. Michael Decter, the former chair of the Health Council of Canada told the CBC that because Canada’s system is public, “we tend to ration everything.”
Across the G7, governments have reduced hospital capacity to cut costs and because advances in medical care have decreased the amount of time patients spend in hospitals. However, older people – who are more likely to spend time in hospital – are also taking up an increasing share of G7 populations. The result is higher wait times, lower surge capacity, and worsening patient care.