Trending Now
We have updated our Privacy Policy and Terms of Use for Eurasia Group and its affiliates, including GZERO Media, to clarify the types of data we collect, how we collect it, how we use data and with whom we share data. By using our website you consent to our Terms and Conditions and Privacy Policy, including the transfer of your personal data to the United States from your country of residence, and our use of cookies described in our Cookie Policy.
{{ subpage.title }}
COVID-19 holiday update: The latest on the Omicron variant
COVID-19 holiday update: The latest on the Omicron variant
Daily coronavirus infections in the US reached an all-time high this week, with nearly 484,377 confirmed new cases on Wednesday alone. Several European countries including the UK, France, Italy, and Spain are also setting pandemic records. Public health officials are blaming the sharp spike in cases on the rapidly spreading Omicron variant.
The last time I wrote about Omicron was on December 3, only weeks after the strain was first discovered in South Africa. There was a lot we didn't know about the new variant back then, but tons of new data has come out since.
To get you a lowdown on this latest stage of the pandemic, I sat down with Eurasia Group's top public health expert, Scott Rosenstein. Our conversation (lightly edited for clarity) is below.
Omicron first crossed our radar in late November. At the time, we heard “in two weeks we will know more,” and it’s now been about four weeks. Do we know more?
Yes we do. Particularly for two out of the three big questions (transmissibility, vaccines, severity).
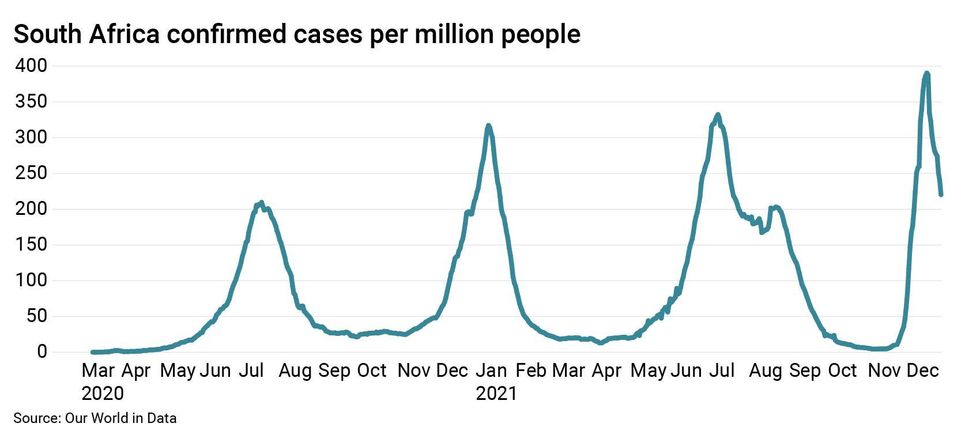
On transmissibility, we know that Omicron is spreading really fast. In South Africa, the case curve had a steeper upward slope than any of that country’s previous waves. But there wasn’t a lot of Delta (or any other variant) around during that outbreak, so it was hard to tell what Omicron would do when it faced off against Delta.
Want to understand the world a little better? Subscribe to GZERO Daily by Ian Bremmer for free and get new posts delivered to your inbox every week.
Now we know. Omicron is quickly outcompeting Delta in North America, Europe, and likely many other parts of the world in the coming weeks.
On vaccines, what was once an expectations-defying story has been downgraded to just a very good story. If you think back to 2020 B.V. (Before Vaccines), you may remember that many experts said the best we could really hope for was a vaccine that greatly reduced the risk of severe illness and death. Stopping asymptomatic or mild infections was considered unlikely. Then the mRNA trial data was released, those vaccines were rolled out in a number of countries, and the vaccines not only reduced the risk of going to the hospital, but they also prevented people from getting infected and transmitting the virus to others.
In moderately vaccinated countries, cases plummeted alongside hospitalizations and deaths—until they didn’t. As time went on, protection from severe illness remained high while more mild breakthrough cases started to emerge—first with Delta, and now much more so with Omicron.
So the vaccines are still doing what we hoped they would do in 2020, but that early 2021 vaccine euphoria is getting dampened—a lot of vaccinated people are testing positive, typically with mild illness. And higher risk people (the elderly, the immunocompromised, those with underlying conditions) that have been vaccinated are still sometimes getting severely ill (albeit less frequently than before). Most concerningly, Omicron is incredibly good at finding unvaccinated people, so even in moderately- to highly-vaccinated places, the risk of overwhelmed hospitals remains elevated.
But isn’t Omicron causing more mild illness?
The question around illness severity for Omicron remains the trickiest and most contentious. But we do know more than we did a few weeks ago. The news is relatively positive but still a little difficult to parse.
From lab studies, there is evidence that Omicron isn’t as good as previous variants at replicating in the lungs, where severe illness is more likely to occur. And from real-world data, we can be pretty sure that South Africa’s Omicron outbreak is causing less hospital strain and fewer deaths than previous spikes did. There are some positive signals coming out of the UK as well, but it is earlier days there, and the hospitals are already strained due to widespread Delta transmission.
But the oft-repeated caveat still stands: “A small portion of a very large number is a large number.” In other words, Omicron is spreading far and wide and causing at least some severe illness and death, suggesting that a raging outbreak that spreads faster than ever could still put a serious strain on hospitals in the coming weeks, particularly if the most optimistic scenarios are overstated and Omicron hits healthcare workers already pushed to the brink.
And it is still difficult to ascertain whether the positive real-world data is due primarily to more people having protection from vaccination and/or recent infection, or to the variant being “intrinsically” less severe than its predecessors and therefore less of a risk to the immunologically naïve (i.e., people who haven’t been infected or vaccinated). The answer to this question is not merely academic—if this variant is as dangerous for the unvaccinated and uninfected, the damage around the world could be severe, particularly in developing countries with little ability to cushion the economic blow of more outbreaks and restrictions.
Can you at least tell me when this wave will end?
This variant seems to be on a super-charged timeline, as the time from infection to symptoms and transmission seems faster than previous waves. In South Africa, just as the way up was very fast, so was the way down. And it’s possible we will see something similar in Europe and the US. But it’s unlikely it will all happen in tandem.
Importantly, more bumps in the road aren’t out of the question—the most concerning of which is the record-setting level of pediatric hospitalizations we’re seeing in parts of the US. Headlines around this story are definitely troubling: if this virus turns out to be hitting children harder than before, that would be a gamechanger.
Of course, context is important. Some of these trends started before Omicron, and hospitalizations are still overwhelmingly in unvaccinated children. So it may just be evidence that this outbreak is larger than ever in this group due to the resumption of pre-pandemic behavior. In other words, risks for children may be the same and still considerably lower than for adults, but the outbreak is now so large amongst this mostly-unvaccinated cohort that we’re going to see spikes in hospitalizations like we’ve never seen before.
Regardless, we’re seeing unprecedented case numbers across all age groups, and record-setting holiday travel suggests this pattern isn’t going to reverse itself just yet—even if that isn’t always reflected in official numbers due to testing shortages in places like the US.
What about the new treatments we keep hearing about? Could those put a definitive end to this nightmare?
Help is certainly on the way in the form of more treatments that are easier to administer than previous treatments like Remdesivir and monoclonal antibodies. Paxlovid from Pfizer remains the best hope for cases that are identified early, which adds even more urgency to solving the current testing shortages in the US.
Supply will be limited in the coming weeks so we probably won’t see these treatments make a big dent in the current surge. By late January, however, that could change. And it could be a harbinger of things to come in many countries around the world as they manage the bumpy transition to “living with the virus.”
New treatments like Paxlovid plus more vaccinations plus protection from previous infection could equal less strain on hospitals and a transition from a state of emergency to a long-term disease management approach to Covid.
Not every country will reach that point at the same time—emerging markets with low to moderate levels of vaccination and limited access to new treatments will once again be at the back of the line. And projections around this built-up wall of immunity have been proliferating for many months now, and they’ve been wrong every time (remember when Sweden was going to hit herd immunity in May 2020?). This time very well could be different. But surprises can’t be ruled out, as much as we all wish they could.
Could Omicron end up being a good thing?
It depends entirely on your time horizon.
In the short term, with hospitalizations still rising and all sorts of economic disruption mounting (e.g., massive flight cancellations), it’s hard to see this Omicron surge as anything but a bad thing.
In the medium term, it’s quite possible that this really does turn out to be the “exit wave” that we’ve discussed numerous times before, particularly for highly vaccinated countries. If Omicron is able to totally outcompete Delta (which remains uncertain) and turns out to be a much smaller threat to healthcare systems, then Omicron could ultimately be a good thing.
What would need to happen for the US to go back into strict lockdown?
A time machine to take us back to early 2020? A massive Ebola outbreak? Other than that, it’s hard to imagine most states going into anything resembling a strict lockdown.
At the peak of the US response in March/April 2020, even the strictest states only imposed “soft lockdowns” compared to what other countries did. In blue states, if you had parking lots filling up with very young Covid patients, you could imagine the return of indoor capacity restrictions, more mask mandates, hybrid education, etc. None of that really qualifies as a lockdown. China’s response to outbreaks qualifies as a lockdown.
Overall, pandemic fatigue is very high and the appetite for restrictions remains very low across much of the US. I don’t see that changing as we enter the third year of this pandemic.
Speaking of China, I’ve seen some data showing that even 3 doses of Sinovac might be ineffective against Omicron. What would this mean for China and for the global economy?
Sinovac does appear to be ineffective against infection. But it’s a difficult question to answer at this point because we still don’t have a great understanding of what that means for severe illness. Right now it’s probably safe to assume that these vaccines will be at least OK on this front but a little less OK than other vaccines on the market (similar to what we saw with Delta).
Even small differences in effectiveness would mean that countries that have been relying on Sinovac vaccines could see more explosive case spikes than those depending on mRNA vaccines (which are already seeing case spikes of their own due to reduced effectiveness against infection and transmission). This could once again strain hospitals in countries with already limited healthcare capacity (e.g., Indonesia). Many countries had already been diversifying away from Chinese vaccines for exactly this reason, and this data—if confirmed—will continue that trend.
In China, it means that the vaccines themselves won’t do much to stem a potential Omicron surge, meaning Beijing will continue to rely on its stringent “Zero Covid” strategy. This approach was always more focused on “NPIs” (non-pharmaceutical interventions), so Beijing will stick with that until it’s at least able to stock up on enough mRNA boosters and treatments like Paxlovid that can further reduce the risk of severe illness. That’s likely a number of months away. And the 20th Party Congress will convene in October 2022. Beijing has touted its Covid success as an example of its superior governance philosophy, so even small outbreaks before then are going to be seen as politically unacceptable, meaning risks of social and economic disruption in China—and therefore the global economy—will be with us for much of 2022.
🔔 And if you haven't already, don't forget to subscribe to my free newsletter, GZERO Daily by Ian Bremmer, to get new posts delivered to your inbox.